Megan’s strength was deteriorating rapidly. We had taken our final last dance a day before. Megan now needed to be helped to a wheel chair to make the approximately 14-feet trip to the porch from the hospice bed in our living room. Once there, I stood behind her and caressed her head, as I steadied her now-weak neck, so that she could look ahead at our neighborhood and admire our porch.
Earlier today Megan’s feet began developing splotches of blue. I knew this meant her circulatory system was having trouble getting oxygen to all her extremities. We frantically massaged her feet in an effort to encourage blood flow and saw an improvement in skin color. Daisy later told us that the coloring was normal at this point in Megan’s care, and that our massage was actually not a good idea as it could ultimately result in the dislodging of a blood clot that could race through Megan’s body, and potentially cause an embolism. Fortunately this did not happen, but this was a difficult reminder of how severe Megan’s condition was, and that we needed to be mindful of so much and rely on the hospice assistance.
The Lactulose was now working. It was working too well. Megan’s deteriorating strength made this more difficult and ultimately this drug would prove to be an exercise in futility. Her cognitive ability only deterioated, and the expedition in bodily function ultimately contributed to distress in Megan’s last days. As we would roll, and reposition and clean Megan, each towel-stroke or touch began leaving bruises, no matter how gentle we tried to be. Megan’s body was shutting down.
As the sun shown down on us, the large contrast between this trip and our Hurricane Irene-break was apparent. There was no need for the warmth of Jennifer’s shawl under this 70 degree summer-like day. Instead, Megan and Jocelyn recreated a moment straight from their childhood as they lovingly shared a sugary ice-pop bite-by-bite. A debate about how best to handle the watery-syrup mix at the bottom ensued. Although Megan did not speak up to participate, I’m sure one of the sun-splashed smiles she showed was an approval in response to this banter and it’s conclusion.
At the outset of this porch trip, some co-workers of Megan’s arrived to visit. We helped Megan back inside and left her and her colleagues alone to speak. As I write this, I’m reminded of the last time Megan spoke to her boss prior to seeing him on this day.
Megan called Jeff from the hospital a day or two before we really understood what was happening. At this point there were still many reasons to hope and expect that Megan would exit the hospital and resume some semblance of normalcy, but she knew her time at work was numbered.
Megan described the state of the project she was working on. After disclosing the location of her source-code, notes and similar, pertinent details, Megan painfully reflected on her time on this project. She was clearly disappointed that she would not complete it, almost to the point of being apologetic.
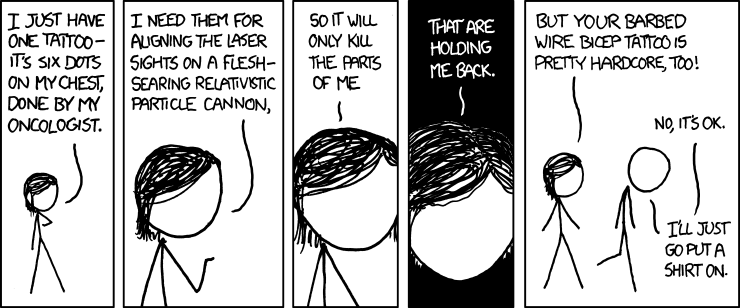
Throughout her life, Megan had a natural desire to see everything to it’s end in the best possible way. She had a desire to succeed at the highest level with everything she did, and this battle was no different. Her first medical oncologist, Mr Wizard, described Megan as a ‘firecracker’ and said her ‘normal’ was about 120% of how the rest of the us are. Megan also described in this blog several times her desire to be at the "top-of-her-class" among the studies conducted by her most-recent (and adored) oncologist.
In the 1200+ days from her original diagnosis, I think this was the first time that Megan allowed herself to relinquish some significant bit of control of something to cancer. And even then she was still confident and unrelenting. As she spoke on the phone in the hospital room, she ended her call with Jeff saying that that she would log-in remotely and take care of some final tasks - just as soon as she could.
Megan never gave up.